Published March 29, 2022 | Updated February 8, 2024
By MedCourse
Useful, relevant, and interesting content for UK Junior Doctors.
Have you ever sat in a medical handover, exhausted following 12 hours of extinguishing fires across the hospital, and listened to the conversation between medical trainees thinking “I have no idea what is happening”?
You’re not alone.
Internal Medicine Training (IMT) is the 3-year UK programme that aims to turn you from that dumbstruck foundation trainee into the legendary medical registrar – a hardened veteran of the acute take, master of the dumping grounds, wizard of the wards.
The “Internal Medicine Trainee” badge on your lanyard may still draw raised eyebrows from colleagues who had only just gotten their head around Core Medical Training (CMT), but with a transition to IMT in 2019, there’s still confusion over what an IMY1-3 is.
In this ultimate guide to internal medical training, we will walk you through what the training programme is, the curriculum and what life as an IMT is like.
Justin, Priyanka, and Sashi have generously contributed to this article with their tips, advice, and experience. They all aced their applications and work with Optimise Interviews to help applicants nail their IMT Application and Interview.

Justin studied medicine at the University of Edinburgh and did his foundation years in Scotland, during which he successfully completed a part-time MSc in Clinical Education.
He subsequently moved to the Northwest to continue his training as an NIHR Cardiology Academic Clinical Fellow, and IMT.

Priyanka studied Medicine at the University of East Anglia. She enjoys teaching and pursued an intercalated degree in Medical Education at the University of Leeds.
Now she teaches in various capacities from face-to-face to online-based platforms. More recently, she has started as an IMT 1 trainee in the North West.

Sashi studied Medicine at Cardiff University. Following graduation, he completed the academic foundation programme at Imperial College London.
He enjoys teaching and has completed a PgCert in Clinical Education at the University of Edinburgh, leading a 9-month international teaching programme.
If this advice is useful, you should also check out the Optimise IMT course to help you nail your IMT application.
IMT in a Nutshell
IMT is a 3-year core training program for UK junior doctors, preparing trainees for life as a medical registrar and beyond. Internal medicine UK training comes after the completion of foundation training and leads to higher medical speciality training (ST4+).
You may have heard rumours about life as a core medical trainee. Claims of endless service provision. Frustrations about the day-to-day Groundhog Day of an SHO. Difficulties finding an opportunity to learn.
While unprecedented demand on NHS services means that the 2019 overhaul of medical training doesn’t fix all these problems, the new program aims to address some areas of frustration.
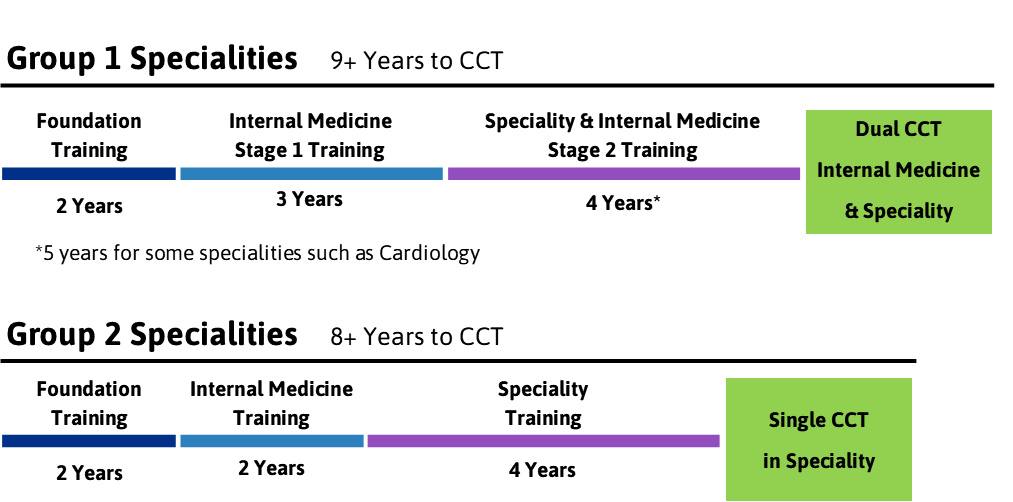
IMT replaced Core Medical Training (CMT) in 2019 and is designed to give medical trainees the opportunity to dual CCT with Internal Medicine – meaning a group 1 speciality consultant can partake in the acute medical take.
The new programme also brought about changes to reduce the “tick-box” portfolio burden, provide support in the transition to becoming a medical registrar, and increase exposure to outpatients, intensive care, and geriatrics.
Internal Medicine UK Training lasts between 2 and 3 years, depending on which speciality you choose to enter. You don’t have to choose how long you will stay in the program when you start – it’s a decision you can make in your second year (IMY2).
Medical trainees who apply to train in group 1 specialities, which dual CCT with the speciality and general internal medicine, must complete all 3 years. Those who wish to apply to group 2 specialities may leave after 2 years and will go on to attain a single CCT in their chosen specialities.
Internal Medicine Training is a hospital-based medical training program. At least 2 years of the 3-year program must be ward-based, though the new programme also requires outpatient clinic experience throughout all three years.
IMT medical rotations are made up of hospital-based inpatient specialities, outpatient-based medical specialities, and intensive care. Geriatrics is a mandatory placement, and most out-of-hours work will be focused on the acute medical take (though the dreaded ward cover will also rear its ugly head depending on your trust).
By the end of IMY2, trainees will be expected to take on the role of the medical registrar, albeit with more supervision than ST4+ equivalent registrars. In their IMY3 year, they will be expected to take leadership roles in ward work, the acute take, and resuscitation teams.
During training, you will be taught to perform procedures including chest drain, central lines, and lumbar puncture. Regular teaching will be delivered by the training deanery, including mandatory simulation sessions.
Trainees are expected to pass the MRCP (UK) exam by the end of year 2 to obtain a satisfactory ARCP outcome. Compared to CMT, this provides some leniency to those who haven’t passed the MRCP by year 2.
You will be allowed to continue their progression without passing MRCP by year 3 (with potential changes to their training and timeline of completion dictated by their deanery), whereas CMTs of old ended up missing out on a ST3 posts due to missing MRCP passing deadlines.
After completion of 3 years of training (2 years for group 2 specialities), trainees are expected to apply for higher speciality training.
Higher Medical Specialities
Group 1 Specialities
Requires Completion of IMY3. Results in Dual CCT with General Internal Medicine.
- Acute Internal Medicine
- Cardiology
- Clinical Pharmacology & Therapeutics
- Endocrinology & Diabetes Mellitus
- Gastroenterology
- Genitourinary Medicine
- Geriatric Medicine
- Infectious Diseases (except when dual with Medical Microbiology or Virology)
- Neurology
- Palliative Medicine
- Renal Medicine
- Respiratory Medicine
- Rheumatology
Group 2 Specialities
Can be Started Following the Completion of IMY2. Results in Single CCT.
- Allergy
- Audio vestibular Medicine
- Aviation & Space Medicine
- Clinical Genetics
- Clinical Neurophysiology
- Dermatology
- Haematology
- Immunology
- Infectious Diseases (when dual with Medical Microbiology or Virology)
- Medical Oncology
- Medical Ophthalmology
- Nuclear Medicine
- Paediatric Cardiology
- Pharmaceutical Medicine
- Rehabilitation Medicine
- Sport and Exercise Medicine
Application for IMT is done online via the Oriel application system, with applicants scored on categories including publications, teaching experience, and quality improvement projects. Your application score will determine whether you are invited to interview. IMT medical interviews are de-centralised, with your interview score turned into a ranking that determines whether you receive your preferred placement.
Trainees can apply for less than full-time training (LTFT) for circumstances that satisfy category one, category two, or category three conditions. You will not need to apply to specific LTFT posts and can make the decision to apply for LTFT during your training. LTFT trainees are expected to work at 50 to 80% of the full-time hours, including out-of-hours work.
Category three LTFT conditions, which allow LTFT training for any personal reason, were introduced in August 2022. Any junior doctor can apply for LTFT, though approval is not guaranteed and must be agreed with the training deanery.
Should I Do IMT?
If you love the buzz of managing acutely unwell patients and the idea of becoming a medical detective, then internal medicine training might be right for you. If you don’t love any of those things… it might also be for you.
Ultimately IMT can be a 3-year love affair or just a means to an end – it depends on what you want to get out of it on the other side.
Thus, the main reason for applying is so you can apply for your higher medical speciality of choice on completion of the programme. Even if you’re not pumped to spend 2-3 more years on the wards, you might just need to put your head down and get to the other side in the best position you can.
On the other hand, core medical training can also be an amazing opportunity to equip yourself with the skills to deal with whatever comes through your door. The journey from a lowly foundation doctor can be challenging, but the reward of becoming the go-to medical advice hotline brings some satisfaction.
With the ageing population, an overstretched health system, and a trend toward super-specialised consultants, core medical training aims to equip consultants with the skills to deal with a broad range of medical conditions and provide more holistic patient care.
You may relish the challenge if you enjoy:
- Clinical problem solving
- Team-based hospital environments
- Hands-on ward-based procedural skills
- Attention to detail when examining and investigating patients
- Managing both chronic conditions and acutely unwell patients
- Leading teams day-to-day and during emergencies
- Working closely with most other specialities
Another important factor to consider when deciding whether to pursue medical training is work-life balance. Whether you’re planning to continue working as a medical registrar or to apply to a group 2 speciality, weekends and nights will feature in your rota.
Major changes from CMT to IMT
Core Medical Training (CMT) was the post-foundation training programme for medics prior to 2019, leading on to ST3 higher medical speciality applications. It’s no secret that Core Medical Training had a reputation problem. Core medical trainees were often disillusioned with the tick-box nature of CMT, and a sizeable chunk of CMTs required extra time to complete their training or pass exams before becoming a medical registrar.
Another reason for the change from CMT was that, with increasing specialisation and sub-specialisation of medicine, deaneries were concerned that newly qualified consultants might not be able to provide holistic care to an ageing population with increasingly complex health needs.
In August 2019 UK core medical training was overhauled. Core Medical Training (CMT) became Internal Medicine Training (IMT) and was extended from 2 to 3 years duration. The extra year of training was used to give trainees (who don’t leave after the second year for group 2 specialities) a chance to work as a medical registrar with an increased level of supervision.
This change was also designed to increase the number of consultants with a general internal medicine CCT who could partake in the acute medical take.
Summary of Changes
- An increase in program length from 2 years to 3 years (for those applying to group 1 higher specialities only).
- An increase in the number of specialities requiring completion of post-foundation medical training prior to higher speciality training application.
- An Intention to reduce speciality training (ST4+) from 5 years to 4 to compensate, though for some specialities this might not be the case e.g. Cardiology.
- Increased supervision and support in the transition to becoming a medical registrar in Internal Medicine Year 3 (IMY3).
- An option to delay the transition to medical registrar (due to issues with competencies or MRCP exam) without extending training.
- A greater focus on managing complex and comorbid patients, as well as more support in managing acutely unwell patients in IMY3.
- Mandated experience in critical care, outpatient clinics, and geriatrics.
- The replacement of the CMT tick-box list of conditions for portfolio with a more generic “capabilities in practice” model.
With the new core training programme, medical training is designed to better prepare the trainee for life as a medical registrar and beyond – though it’s yet to be seen whether old grievances will continue despite changes to the programme.
The IMT Curriculum
The IMT curriculum includes targets for trainees to on medical conditions seen, procedures performed, and more generic “capabilities in practice” completed.
With the implementation of the new programme in August 2019, the Joint Royal Colleges of Physicians Training Board (JRCPTB) has made several changes to the curriculum of UK core medical training.
The curriculum aims to equip trainees with the skills to:
- Provide safe care in emergency and acute medical scenarios
- Manage complex acute and long-term medical conditions
- Communicate effectively with patients and relatives
- Become a senior decision-maker in the management of medical patients
- Lead medical teams and provide support to junior colleagues
The curriculum is based on capabilities in practice (CiPs). Trainees will need to provide evidence via their e-portfolio to prove they have met these learning outcomes satisfactorily.
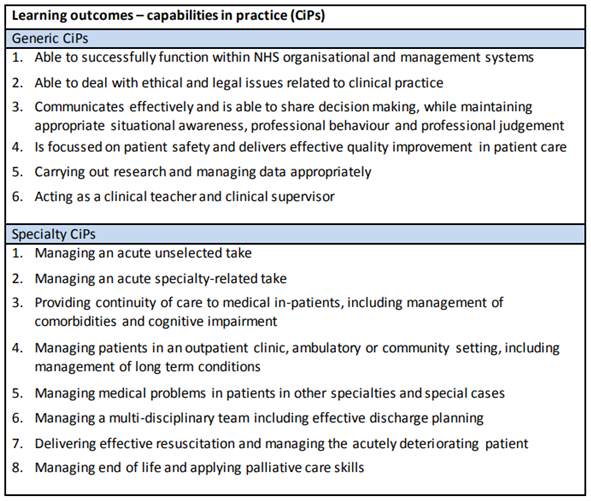
Evidence for these CiPs can include consultant feedback, work-based assessments, supervisor reports, logbooks, and reflections.
Before August 2019, the Core Medical Training (CMT) curriculum included a “tick-box” list of conditions for which the trainee required evidence of competence. The IMT curriculum has moved towards more generic competencies, but still has a list of key presentations and conditions which are included in the syllabus.
In addition to presentations and conditions, trainees are expected to learn and demonstrate competence in some core practical procedures. These are generally ward-based procedures that they would be expected to perform as part of their role as a medical registrar. Most procedures are required to be performed on real patients, whereas some can be performed in the skills lab.
IMT Core Procedures
By the end of IMY2 the trainee should be competent to perform each procedure unsupervised. Procedures include:
- CPR
- Temporary cardiac pacing using an external device (skills lab minimum)
- Ascitic tap
- Lumbar puncture
- Nasogastric tube
- Pleural aspiration for fluid
- Femoral IV or interosseous access*
- Central line – internal jugular or subclavian*
- Chest drain for effusion*
- Chest drain for pneumothorax*
- DC Cardioversion
- Ascitic drain – abdominal paracentesis*
*Can be performed in a clinical skills lab environment.
The curriculum also includes targets on patients seen on the acute medical take, outpatient clinics attended, and experience in specialities including geriatrics, critical care, and palliative care. Learn more about the ARCP requirements below.
Getting Through IMT
So how do you go from that lowly FY2 to the first person they call when they’re in trouble?
By the end of your core medical training, you will possess all the skills to be a fully grown medical registrar. You will have full membership of the Royal College of Physicians, the ability to lead an acute take and cardiac arrests, and the know-how to run the wards day and night.
Training comes in two stages across 3 years. In the first stage, you will act as an “SHO” equivalent, though you might be given more seniority and leadership roles than you did as an FY2 doctor. In the third year of training, pending completion of MRCP(UK) and meeting your educational supervisors’ expectations, you will act as a medical registrar, albeit with additional supervision.
IMTs starting the programme will have different levels of experience, including:
- Trainees who have entered the programme immediately following foundation training
- Those who have undergone one or many “FY3 years”
- International graduates who have gained foundation competence following training in another country, some for many years
- Doctors who trained in other specialities but since decided to join the IMT programme
You might have peers who have already acted as a registrar outside of training, colleagues who seem to have an encyclopaedic knowledge of almost every topic within medicine, and team members who exude confidence and competence to their core. The important thing is to focus on your own progress, rather than on your peers.
Throughout the programme, you will rotate through different medical specialities, both inpatient and outpatient-based, generally on 4- or 6-month placements. It’s likely that you’ll be expected to partake in on-call duties throughout your training, including weekends and nights.
Internal Medicine Training Year 1 (IMY1)
In the first year of IMT you are expected to start your professional development beyond what you have achieved in FY2. The focus of this year is on inpatient medicine, so you’ll be spending a lot of time on the wards.
The ARCP at the end of IMY1 (year 1 of core training) is not a critical progression point, so if you miss out on a few key requirements it might not affect you progression. It’s a good idea to use your IMY1 wisely though to make sure your IMY2 isn’t overwhelming.
It’s wise to start preparing for MRCP(UK) exams as soon as you’ve found your feet in IMY1. MRCP part 1 is an exam with which many doctors struggle with and require multiple attempts. MRCP part 2 PACES can also be a massive undertaking and should be signed off by the end of IMY2, so if you can pass your part 1 and part 2 written early you’re giving yourself plenty of time to prepare.
If you have placements in IMY1 which are within the same trust as IMY2, this is a good time to begin a quality improvement project (QIP). You’ll need to perform more than one cycle of your QIP by the end of IMY2, so by starting off in a trust you’ll be back at later, you can avoid late-night drives across the region to meet ARCP deadlines.
IMY1 is also a good time to start ticking off the core procedures required, as in IMY2 you are likely to spend less time on the wards. Show some enthusiasm on the wards and tell your registrar which procedures you’d like to get involved in. Medical registrars have been through the same scramble to tick off all the procedures, so are likely to show some empathy and give you a call when an opportunity pops up.
Internal Medicine Training Year 2 (IMY2)
In the second year of IMT the focus starts to shift towards outpatient medicine. Unfortunately, you’re still in the “SHO” category at this stage, and with an overwhelmed NHS system you’re going to face difficulties meeting ARCP clinic requirements when the ward is understaffed.
Try to get clinic time early in each placement while the wards are well-staffed. Some educational supervisors will help you by scheduling clinic time, but if not you’ll need to emphasise its importance and push to get off the wards when you can. Twenty clinics in one year doesn’t sound like much, but if you’re not proactive you might struggle to meet the ARCP deadline (typically between May and July).
In addition to attending clinics, it’s also time to complete the QIP you started in IMY1 or complete a whole new one. Six-month placements sound like a long time, but if you don’t tell your supervisor that you want to perform a QIP at the start of the placement, time may get ahead of you.
You’ll also want to cosy up to some consultants who you work with on the acute take, as you require three consultants who have personally supervised you on the acute take for your Multiple Consultant Reports (MCRs).
This year’s ARCP is crucial to progress as expected into IMY3. The new curriculum was designed to give more time to trainees who needed it before becoming a registrar, and if you don’t get a good ARCP outcome you might be stuck acting as an SHO for some of your IMY3.
By the end of IMY2 you’ll be expected to have passed the full MRCP(UK) exam, though some allowances will be made for those who haven’t. As this is an “outpatient” year, you should make the most of inpatient speciality rotations to search for PACES patient cases and work with others who are revising for PACES.
Engage with your local department as much as possible!
I know the nature of rotational training doesn’t always lend itself well to this, however, in my experience even with a short amount of time, if you stand out as a keen and engaged junior, more opportunities become available to you.
As an example, I am keen on cardiology, so in my rotation, I made it known from the off to my educational and clinical supervisors and made a very conscious effort to attend as many M&M, journal clubs, echo case presentations, departmental teaching (both junior and senior!) and even managed to negotiate some time off wards, whilst it was well staffed, to shadow the on-call cardiology registrar.
This was beneficial as it not only gave me exposure to the speciality but opened many opportunities to get involved in stuff that will help in applications. In a 4-month rotation, I was able to work with one of the Heart Failure consultants in my trust to audit current local prescribing practices, update our local guidelines and re-audit, resulting in a 2 cycle QIP as well as a national poster presentation at the British Cardiovascular Society.
Lastly, whilst this can be difficult (and I still struggle with this as an IMT trainee at times), try not to get disillusioned about the ward jobs and try to focus on the unique speciality aspects of a rotation which will be more of what you do on a day-to-day basis once you are beyond the FY/IMT years.
Internal Medicine Training Year 3 (IMY3)
This is an important year for IMTs. You’ve spent the past two years preparing, have ticked all the right boxes, brown-nosed all the right people, all so that you can…
…get a big pay rise!!
In all seriousness, IMY3 is your time to put theory to practice and begin your life as a medical registrar. The extra money isn’t going to come without a few strings attached! If you have shown competence and ticked all the boxes in your IMY2 ARCP, this is the first time you’ll be able to call yourself a registrar.
Don’t be too scared. Medical registrar sounds like a big and scary job to foundation doctors, but after two years of training, you’ll realise that you know more than you thought. You’ve passed all the difficult exams, know how to do all the procedures, and have some time in critical care under your belt.
The difficulties of becoming a medical registrar are in the details – should this patient be for escalation? Who can I safely step down from a monitored bed to make room for the unwell patient in ED? Should I wake up the consultant to discuss this ICU admission?
IMY3 is designed to be a supported transition to life as a medical registrar, so you won’t have to deal with all of this by yourself. Deaneries will ask hospital trusts to give increased supervision to IMY3 registrars – generally through an additional on-call registrar or a guarantee of consultant backup.
Other than the step up from being an SHO, you will also be expected to demonstrate leadership in QI activities, as well as attend more clinics than in the previous two years.
The good news is that as a registrar you might finally be able to delegate discharge summaries!
Worth it.
Study Leave & Courses
As an Internal Medicine Trainee, you will have more study leave so that you can attend courses and prep for exams. You will have 30 days of study leave per year, though the actual number will be smaller after any mandatory IMT training is deducted. Most deaneries will allow for days off prior to an exam as “private study time”, but this is likely to be limited to a week or less of your total budget.
As soon as you start a new rotation you should start planning study leave. The later you plan for this the less likely you’ll get it, as your colleagues start to put in their own leave requests. Study leave is an amazing way to get away from service provision and learn, as well as an opportunity to improve your CV in time for higher speciality applications.
Compared to FY2 you’re likely to get a bigger study budget, though this depends on the deanery. Study budgets have become centralised by HEE recently, meaning you can spend as much your educational supervisor and training programme director agrees is appropriate, though your deanery may still place a hard limit on spending.
Even if your course costs more than your study budget, you might still have a chance to reclaim the money. Study budgets are notoriously left unspent, so come January your TPD will be trying to get trainees to either book new courses or claim extra money from previously attended courses before the deadline at the end of March.
So, what should you spend your study budget on? It might be a little predictable of us to say, but courses!
Attending a course as an IMT can have so many benefits:
- Earn more application and interview points for your speciality application
- Learn new skills from experts with better experience and equipment than your local skills lab
- Take time off from ward service provision and learn in a calm and stress-free environment
- Show commitment to speciality in time for higher speciality application
Looking back, you get very little study leave in FY years (it gets better in IMT but in FY you hardly get any) and so I wish I’d done more of this as a student.
I really enjoyed going to a medical trainees conference, as I learnt lots that interested me in this massive speciality and met more motivated people! This cemented my decision to apply for IMT!
My Takeaway would be that even if you are not sure about the speciality, go on a related course (I went on a career in radiology course that my hospital was offering). Although it wasn’t for me – I would never have realised if I had not taken the lead to go on this course.
One final tip I can give is that while I know money can be a limiting factor if you find a course that will help your career, you should view it as investing in your education. If you go to a conference that turns into a future PhD, or if you go on a course that gets you the dream job you want, then it is worth every penny – but it is hard to view it like that before you attend.
Often many hospitals have dedicated pots of money for Fellows to attend courses and conferences. These are not widely advertised but usually the training program director or the manager responsible for the rotor. Will know how to access this. It may involve filling in a few forms but if that gives you a free course it is definitely worth it.
Clinical Seminars, Workshops, and Courses
You know what your weaknesses are, and which specialities you’re struggling with. You might be able to get through training safely without putting in extra time that’s great, but if you’re really feeling the gap in your knowledge what better way of learning than taking a day to listen to experts?
Another fantastic reason for attending clinical update courses is to show your commitment to speciality. For competitive higher medical specialities, you need to stand out and show that you’re serious, so attending a speciality-specific seminar, workshop, or course can give you that boost you need.
These clinical courses can include:
- Speciality-specific Clinical Courses
- Clinical Update Seminars
- ECG Workshops
- Clinical Skills Workshops
Exam Courses
MRCP(UK) courses can be vital to pass these difficult exams. Traditionally most courses focus on PACES but given the high repeated fail rate of part 1, there are an increasing amount of revision courses for MRCP(UK) part 1 and 2 written exams.
MRCP(UK) PACES courses are almost seen as a requirement for passing this practical exam. While it’s not absolutely necessary, especially with the advent of online video resources such as Pastest, many of the conditions you’ll be expected to recognise in the exam are rare. PACES courses give the opportunity to see many of these rare cases over the course of a few days, with expert guidance on your examination skills and a mock exam built into the course.
Procedural Skills Courses
Courses are an amazing way to learn a new clinical skill without being asked “Is this the first time you’ve done this?”. To get your core procedures signed off you need to be in the right place, at the right time, with the right senior. If you already know what you’re doing seniors are more likely to watch you do the procedure on your first real patient.
Procedural skills courses can help you learn:
- Procedures such as lumbar puncture, chest drain, and central line insertion.
- Ultrasound skills to perform FAST scans, scan pleural fluid before a drain, or perform ultrasound-guided IV cannula insertion.
- Surgical skills to help in the catheter lab or with your suturing skills. (You never know when it might come in handy!)
Professional Development Courses
By the time you’ve finished IMT, you should have all the skills you need to lead the acute take and deal with patient emergencies. Soft skills on the other hand are much harder to master and aren’t part of the core curriculum.
To get a head start before starting as a medical registrar, book a career skills course:
- Leadership courses help you to manage your team and get the best out of your juniors. Your life as a medical registrar will be so much easier if you can lead your team well.
- Communication courses make difficult conversations with patients and relatives so much easier. So many complaints can be avoided with good communication!
- Interview courses will make you look and feel confident during one of the most important and nerve-wracking moments of your life. If you haven’t been to an interview since medical school, you might be feeling rusty.
- Teaching courses such as teach the teacher get you extra points on your application and give you the skills to educate the next generation of doctors.
Portfolio and ARCP
Portfolio often drops to the bottom of your list when you’re in the thick of it on the wards, but if you leave things to the last minute you’ll end up pulling your hair out trying to tick all the remaining boxes.
The portfolio is completed online and is made up of reflections, supervisor forms, work-based assessments, and other mandatory sections such as clinic logs and quality improvement forms. You’ll need to link your forms up to the curriculum section of your e-portfolio to complete your ARCP goals.
Work-Based assessments include:
- Multiple Consultant Report (MCR) – feedback forms from consultants who have supervised your work.
- Multi-Source Feedback (MSF) – feedback from up to 15 colleagues including peers, consultants, and allied health professionals.
- Acute Care Assessment Tool (ACAT) – clinical skills assessments that summarise your care of 5 patients with the same consultant supervising.
- Case-based Discussions (CbD) – discussion with a senior around a clinical case.
- Mini Clinical Evaluation Exercise (mini-CEX) – supervised patient contact which can involve skills such as history taking and examination.
- Directly Observed Procedural Skills (DOPS) – supervised clinical procedures.
One thing I found useful was saving the Horus ePortfolio web page as a shortcut on my phone home screen.
In FY1 I left my ePortfolio to the last minute and it was really stressful getting it all done in time. So when I started FY2 I promised I would take a different approach and aimed to send 2 or 3 tickets each week.
I would do it straight after a post-take round or doing a procedure so I wouldn’t forget and have all the clinical details to hand.
This was so much better as I had most of my tickets sent out in the first 6 months…and then spent the next 3 months chasing people up to complete them!
The Annual Review of Competency Progression (ARCP) is an evaluation of your progress and takes place a few months before the end of each year.
ARCP is the culmination of any work you have done for your portfolio, with a panel including your training programme director (TPD) and deanery determining if you have met the years ARCP requirements, as detailed below.
ARCP Requirements
| Requirement | IMY1 | IMY2 | IMY3 |
| ESR Report | Meets expectations | Will meet critical progression point to reach IMY3 | Will meet critical progression point to complete IM stage 1 |
| General capabilities in practice (CiPs) | Educational supervisor confirms that all expectations met for stage of training. | Educational supervisor confirms that all expectations met for stage of training. | Educational supervisor confirms that all expectations met for stage of training. |
| Clinical capabilities in practice (CiPs) | Meets expectations. | Meets critical progression point requirements | Meets critical progression point requirements |
| Multiple Consultant Reports (MCR) | 4 | 4 (3 acute take) | 4 (3 acute take) |
| Multi-source feedback (MSF) | 1 | 1 | 1 |
| Acute care assessment tool (ACAT) | 4 | 4 | 4 |
| Supervised Learning Events (SLEs): Case-based discussion (CbD) or mini clinical evaluation exercise (mini-CEX) | 4 (by consultant) | 4 (by consultant) | 4 (by consultant) |
| MRCP (UK) | Part 1 passed | Full MRCP(UK) passed | Full MRCP(UK) passed |
| Advanced life support (ALS) | Valid | Valid | Valid |
| Quality improvement (QI) project | Participation with evidence e.g., QI project started & project plan submitted | 1 project complete | Demonstrates leadership in QI, e.g. supervising another health professional |
| Clinics attended | 20 clinics | 20 clinics | 20 clinics & 80 clinics total over all 3 years |
| Acute unselected take | 100 patients seen | 100 patients seen | 100 patients seen & 500 patients total over all 3 years |
| Rotation requirements | n/a | n/a | 24 months ward-based care 10 weeks critical care 4 months geriatrics |
| Teaching attendance | 50 hours including 20 hours of local “IMT” teaching | 50 hours including 20 hours of local “IMT” teaching | 50 hours including 20 hours of local “IMT” teaching |
What is Standalone IMY3?
Until the 2023/24 application period, standalone IMY3 recruitment was available for trainees who had previously completed core medical training (CMT) or Acute Care Common Stem – Acute Medicine (ACCS-AM) but have not gone into higher speciality training. These trainees could complete the third year of training so that they were eligible for ST4 recruitment.
Recruitment for standalone IMY3 recruitment has now ceased and is no longer available as a recruitment pathway into IMT.
Entry to ST4 training can also be gained via the ‘Alternative Certificate to Enter Group 1 Higher Physician Specialty Training’ form, with more information available on the physician higher speciality training website.