Published July 27, 2023 | Updated August 17, 2023
By Callum Airlie
Trained in Edinburgh with a specialist interest in Emergency Medicine and a wilderness twist. Not afraid to take an unconventional route through specialist training!
If you’re new to the UK, new to medicine or just looking to hone your skills further; I hope this guide will shed some light on the mysteries of the doctors’ on-call shift!
We’ll cover content pertinent to hospital ward cover rather than the emergency department or admissions units as they’re separate beasts entirely and require a different approach. The information in this guide is largely aimed at the evening shifts however the principles and ‘top tips’ are certainly pertinent for night shifts too so please feel free to adapt the information provided!
See my Emergency Department survival guide if this is where you’re headed instead.
Evening and night shifts in UK hospitals tend to be busy! Maybe it’s the reduced staff number, maybe it’s the fact that everything is a little scarier in the dark?
Because they’re busy shifts you see a lot of pathology and you’re often the first person on the scene to start figuring out what’s happening and start treating someone appropriately. They’re actually a fantastic opportunity to learn, get exposure to unwell patients, and sometimes (depending on your rotation) they’re a break from a 9-5 life of discharge letters!
What is an On-Call Shift?
If you’re just landing in the hospital for the first time, especially as an IMG new to the NHS, the term “on-call” might baffle you. The meaning of “on-call shift” can mean different things to different people.
An on-call shift is a period of time during which the doctor is available to provide care to patients at a moment’s notice. On-call shifts are usually scheduled outside of regular working hours, such as overnight or on weekends.
There are two main types of on-call shifts:
Non-Resident On-Call (NROC)
During a non-resident on-call shift, you are not expected to be physically present in the hospital for the whole shift but must be available to come in or give advice over the telephone.
These are almost always related to senior doctors (primarily consultants) and are usually limited to out-of-hours work such as weekends and overnight.
An example of this includes a surgical registrar working in a speciality or hospital that doesn’t provide as much out-of-hours work. They would stay within 30 minutes of the hospital (either at home or in hospital accommodation) and come in if they receive a call to for urgent assessment or surgery.
Junior doctors in England on the 2016 contract should receive an 8% pay bump for taking on this work, as well as additional pay for the amount of work they average during these shifts.
Consultants often perform this kind of work. For example, a psychiatry consultant who is available for telephone advice in the evening or a cardiologist on a weekend pacing rota.
Depending on the intensity, these shifts may be for 24 hours (e.g. they work their normal day hours but are available on-call from 8 am that day until 8 am the following day) but may also be associated with a day off (in cases where the workload is heavier).
Resident On-Call
Resident on-call shifts are the more common type of shift for junior doctors. During a resident on-call shift you are expected to be physically available in the hospital for the entire duration of the shift, though for some specialities such as psychiatry, they may be covering a wider area made up of hospitals and other in-patient facilities.
These on-call shifts can include any time of the day or week, though usually, this means they would take you away from your day job to perform acute and emergency care.
Typical On-Call Jobs for Junior Doctors
On-call duties can differ between speciality and grade but include a mix of duties including one or more of:
Typically you will be expected to carry out a range of jobs while on-call (See the excellent ATSP 2016 booklet), which will differ depending on your level of experience. You will usually be given a bleep or another communication device in order to keep on top of your tasks. Here are some typical calls you may take:
ST3+ doctors may only get involved in the first 3 of these job types, and have a greater variety of calls from outside specialities as well as their juniors and consultants. Generally, the workload will be spread throughout the on-call team, with tasks matched to grade.
Sorry, FY1s, but that means all the “urgent discharge summaries” and warfarin prescriptions will get dumped on you! 😮💨
The Evening ‘On-Call’ Shift Setup
A quick note first of how things tend to be run.
If you’re already clued up on the rough setup on the on-call shift then please feel free to scroll below for the tips and tricks! This explanation is largely aimed to cover evening shifts however some of this content will also apply to night shifts as the principles are very similar.
You’ll almost always continue your evening on-call shift from your regular day unless you’ve been assigned to clerk in new patients for the entire shift.
The On-Call Team
An On-Call team is made up of various grades and its size depends on how much work is typically required. An on-call team can include:
Other disciplines such as pharmacists, physiotherapists (for urgent chest physio), and ODPs are also expected to work on-call shifts but aren’t usually part of a specific speciality on-call team.
The evening team usually consists of:
- Consultant in charge
- One or more Registrars (middle grade)
- A few foundation doctors/SHOs
Of course, larger departments will have larger teams, but this is usually bulked out with more foundation doctors rather than more middle-grade doctors. Occasionally an extra registrar sneaks into the rota! Consultant location varies between being on-site, in theatre (for surgical teams) or they’ll be available from home – this depends on the hospital and the speciality.
Be aware that there are often vacant slots in the rota due to illness or unfilled job posts. These can be filled using locum doctors, but sometimes you’ll be short or will have to rope the consultant in to “act down”.
Team Handover
Each department will typically hold a departmental handover at the beginning and end of each day in a central location. This is the day team handing over to the night team or vice versa.
Prior to the handover starting, there is usually a quick huddle amongst the evening team to make sure everyone knows who’s who, but also allocating doctors to cover specific wards.
Usually, one junior doctor will cover at least 2-3 different wards, so it’s important to know when to pay extra attention in handover!
Middle-grade roles vary from team to team. Sometimes they’re in theatre for surgical specialities, othertimes they’re ‘floaters’ moving around the sickest patients, but usually, they’re allocated their own wards and also field advice to more junior members of the team.

Handover begins! Each ward team will come to handover and present to the evening team. This usually consists of unwell patients requiring a re-review, blood tests that require chasing or fluid reviews (assessing the fluid status of a patient and re-prescribing the next bag).
Each member of the team will carry their own pager or phone to allow them to be contacted by the appropriate wards. Not only do you have a long list of jobs from handover, but you are also the first port of call for new issues that arise – fluids that need reviewing or assessing a newly deteriorating patient for example. Each ward will know the pager/phone number of the doctor assigned to cover them, so don’t go trading numbers spontaneously!
Off you go! Everyone disperses and sees to their responsibilities. As usual, Foundation Year doctors and Clinical Fellows phone the Registrar for advice when needed and the Registrar speaks to the Consultant if appropriate.
You’re entitled to a half-hour break during the evening shift so make sure you get some food, water and most importantly…sit down! Everyone then typically hands over anything left or any patients they’re concerned about to the night team who take over the reins.
Surviving (and Thriving!) on an On-Call Shift
Before we get right into it, here’s some extra advice to maintain efficiency: Keep your colleagues happy by reducing inappropriate workload for the on-call doctor.
What NOT to Hand Over
There are a few things to avoid handing over at 5 pm if at all possible. These include but are not limited to:
Of course, life is unpredictable, and this is especially so in the hospital.
Sometimes if sh*t hits the fan during the day, a drug chart might be missed or a fluid prescription forgotten. Your colleagues will have your back, but please remember that out-of-hours shifts are for emergencies, time pressured interventions, and newly deteriorating patients.
You cover a lot of patients when on call and there simply isn’t the time to write discharge letters for patients you don’t know or to re-prescribe 16 medications because there’s no space left in the chart.
Typically it’s good practice to consolidate and prepare for the next day 30-60 minutes prior to handover to ensure these types of jobs aren’t handed over to the evening team.
8 Tips and Tricks
Now here are the top tips and tricks that I’ve picked up in my time that will help ease your transition and make you a master of the on-call shift.
1. Start a Jobs list with two pieces of clean A4 paper at handover.
Take two pieces of paper, you always need more when you’re away from a store room or a printer!
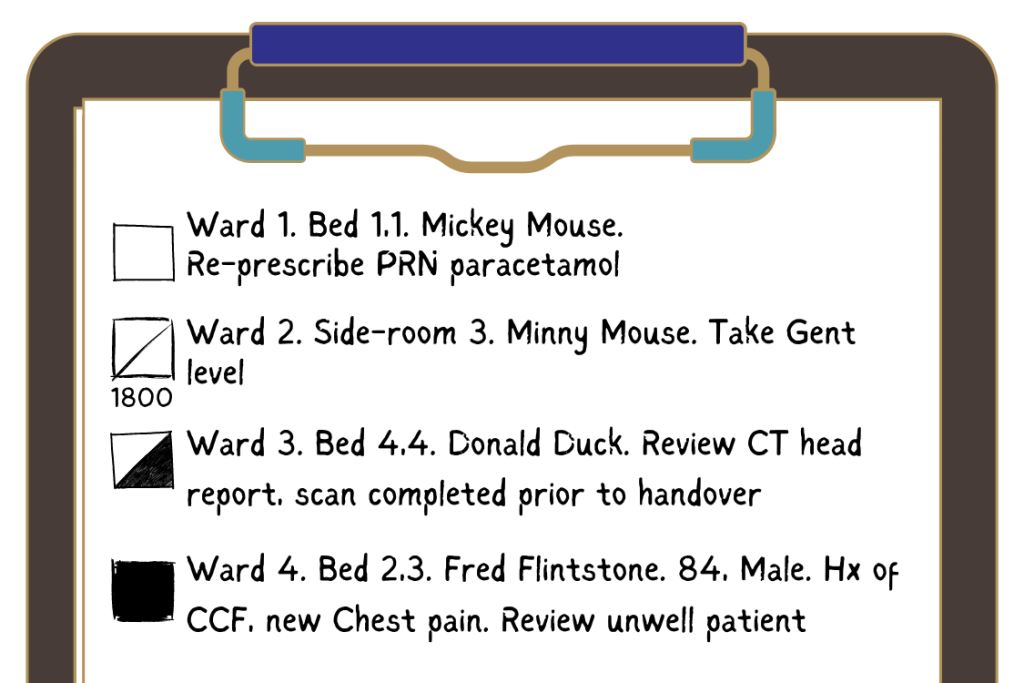
Write down EVERY job, don’t rely on your overstressed memory to keep a job in mind. Be neat, methodical, and have a system. For example, you could always include:
- Ward number
- Bed space
- Patient name
- Brief Info/context
- Task required
- Box to tick
You can figure out your own system for tracking what’s been completed, but here’s the method that was passed down to me:
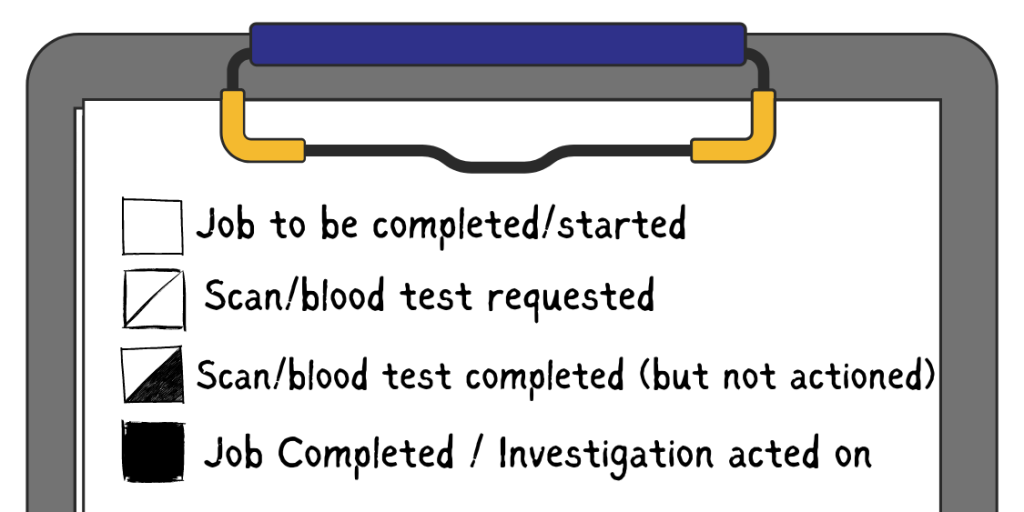
Often it’s useful to have a designated section for each ward. I typically allocate half a page per ward and use the back of the page as extra space for each ward.
Make sure any time-sensitive jobs (fluid reviews at certain times) have the times recorded next to your box; this will be easier to read than the centre of your ‘history’ section!
Example jobs list:
2. Ask for Names and Write Them Down!
This starts at handover. Know who your team are, what their names are and also their grade. Write these down at the top of your handover sheet with their phone/pager number.
When things get stressful and you need help quickly you don’t want to be trying to remember who’s the Registrar and who’s the Clinical Fellow!
This also goes for phone calls about unwell patients or patients suffering falls etc. Take the name AND the bed space and write them down. If the referring nurse doesn’t have the information to hand it’s ok to ask they get it while you’re on the phone.
It’s easy to get bed 3 bay 3 mixed up with bed 3 bay 4 in the middle of the night.
3. Prioritise Your Jobs
After handover, you may have a long list already and it’s easy to get overwhelmed.
Take a step back and prioritise the list either mentally or with little numbers in the margin. Ask yourself “Who will come to harm/the most harm if I don’t do this job first?”
If you don’t need to run to a ward immediately to review someone (this should very rarely be the case), it’s sometimes useful to start the multi-stage jobs first – take a difficult blood test that you will also need to review the result of later.

4. Be Efficient – Keep the Step Count Low!
This is just as important as prioritising your jobs list!
You may spend a significant amount of time walking from ward to ward through this shift and you’ll likely make the same journey multiple times. If there are quick and easy, non-urgent jobs they may be far down your list below patient reviews on other wards.
Don’t be afraid to complete a quick, low-priority job like rewriting an ‘as required medication’ before you run away to the next ward for the unwell patient review.
You’ll get better at judging this as you gain experience. I’m certainly not recommending that you do all jobs on Ward 12 before you walk to Ward 13 if there’s somebody very sick on Ward 13!
However, sometimes by spending just a couple of minutes longer on a ward, you can allow nurses to alleviate pain with another prescription whilst that patient may have waited another 4 hours for you to get to their job on your list otherwise. This one’s not easy and will take time to master, but you’ll get better at judging this over time.
Just remember… there’s no such thing as a ‘quick fluid review’!
5. Don’t Be Afraid to Ask for Help
This works both ways. If you’re sitting pretty with an empty jobs list and having a cup of tea; please, please, please think of your colleagues and give them a call. Better to listen to your conscience than make a mistake.
See if you can do a cannula or take some bloods for them to help with their jobs list. This keeps you available should somebody become very unwell on a ward you’re responsible for, but your team members will always be very grateful! Remember, what goes around, comes around!
Similarly, if you truly are overwhelmed and you suspect you won’t be able to get to jobs as quickly as you safely should, then please don’t be afraid to phone your teammates and ask if they’re available to help out with a job or two.
If their list is full of non-urgent jobs and you have three urgent patient reviews to do it’s certainly more appropriate for them to help out with your jobs! The bottom line is that you must try to prioritise patient safety in any way you can.
You have seniors on the team for a reason! If you have a question or need advice, please phone and ask. It’s always better to ask a safe question than to ignore the voice in the back of your head and miss something important.

6. Take a Step Back and Breathe
Try to periodically stop every now and then and review your list, I always try to do this almost every 90 minutes. This is where it becomes important that you have a clean, methodical, and well-written jobs list.
A quick check through the list makes sure you’ve not forgotten about any time-sensitive jobs, and that you haven’t missed a high-priority job and moved to something else prematurely.
It’s easy to lose track of time and forget the 18:00 gentamicin level you squeezed onto the bottom of page 1. This tip helps you limit your human error rate!
7. Utilise All Members of the Multi-Disciplinary Team
Don’t forget that nurses are skilled health practitioners and you don’t have to complete every aspect of every job yourself!
It’s ok to phone a ward and ask if somebody is available to take a blood test that’s required. They may well say they’re too busy but that’s ok, it never hurts to ask for some support! If you explain your situation and what you’re having to prioritise and juggle, they may be more likely to help out or make a suggestion.
When you take a call to review a patient, it’s incredibly useful to ask questions about history, observations, and investigations already done/requested. Firstly it’s easier and quicker to turn up on the ward to some information but it also allows you to prioritise the review properly!
8. Don’t forget your dinner!
You’re entitled to breaks; Not as a luxury, but to make sure you are working safely and efficiently. It’s very important you eat and hydrate yourself throughout!
Both night shifts and late shifts are less structured and vary dramatically depending on how unwell patients are and how busy you are.
If you’re struggling to get away and carve out your break time try asking yourself “What will happen if I don’t do this job for 30 minutes”.
If no patient will come to harm then that’s your queue to grab some food!

**Other snacks are available.
There you have it.
Follow these tips and tricks and you shouldn’t fall on your face on your first day.
Who knows, you might even enjoy the extra responsibility and start to thrive in the higher-pressure environment?! Best of luck and try to remember to smile!