Published July 24, 2023 | Updated April 16, 2024
By Dr. Maliha Darmini
This is Dr. Maliha Darmini, an IMG in the UK. Trying to balance my medical expertise with the craft of storytelling.
As the world becomes more globalised, it’s no surprise that the medical profession is experiencing an influx of doctors from overseas. Many international medical graduates (IMGs) choose to come to the UK to gain experience and pursue their medical career goals.
However, the journey from being an IMG to becoming a fully-fledged National Health Service (NHS) member can be challenging. In this article, we’ll explore the journey that IMGs go through as they transition to the NHS.
First of all, if you are about to take your very first step towards making a career in the UK, a big CONGRATULATIONS!!! Having a different background, sliding into a totally new culture and also a new system is really a big thing. However, it’s said that “People are not bigger than their DREAMS”.
Up until 2021, the total number of international medical graduates (IMGs) that have paved their way through this journey was around 77,000, with more still coming.
If you want to get yourself into the queue, this article is for you.
About the NHS
Let’s start with a brief introduction.
The journey of the NHS (National Health Service) started in 1948 and is still continuing its legacy as the world’s largest publicly funded health service.
The NHS is a blanket term for three different systems:
Health and Social Care in Northern Ireland was created and is managed separately from the NHS.
They provide a range of health services, free of cost each day with over 1 million patients with respect and dignity. Basically, it’s the 6 ‘C’s The NHS values for high-quality care:
And their core value is “ Patients Come First In Everything We Do”. As an IMG, questions might pile up in your mind about the journey and also various aspects of NHS.
Let’s get a closer look.

Structure of the NHS
The NHS, or National Health Service, is the publicly funded healthcare system in the United Kingdom. It is one of the largest and most comprehensive healthcare systems in the world, and it provides free healthcare to all UK residents.
Treatment in the NHS is free at the point of care for all UK nationals, though those on a visa will be asked to pay a health surcharge of around £624. Free at the point of care means there is no need for payment at any stage of your health journey within the NHS. Private care is still available if you wish to have more personalised care or want to avoid a waiting list.
The NHS is structured into multiple components that work together to provide healthcare services across the UK. The system is responsible for managing healthcare services within its respective region, including hospitals, general practices, and specialised healthcare facilities. The main organisations that make up the NHS are:
The structure of the NHS has changed over time, and it is likely to continue to change in the future. The goal of these changes is to make the NHS more efficient, effective, and patient-centred, though politicians have been accused of using the NHS as a “political football“.
How Patients Interact With the NHS
The way in which patients use the NHS is very different to many other countries, particularly in the way that the majority of outpatient referrals to secondary or tertiary care are handled by primary care practitioners. Here’s the model of how patients use the NHS:
Primary Care
The main-stay of primary care medicine in the UK is via General Practitioners (GPs). The first port-of-call for patients, when they have a non-emergent healthcare need, is generally their registered GP practice.
Medical Practices employ GPs as well as other primary healthcare staff such as:
If a patient has a non-urgent problem that might require outpatient care by a secondary-care speciality, they usually need to be referred by their primary care practitioner.
Other primary care services include opticians, pharmacists, and dentists. These services have their own referral ecosystem whereby they escalate problems which require specialist services.
Emergency Care
When patients have an emergency healthcare need, there are a few options:
Admission to the hospital for emergency care is done via the emergency department, general practitioners (including in urgent care), or outpatient services.
Secondary Care
Secondary care services provide more specialised treatment that is not available in primary care. It is usually provided as part of in-patient and outpatient hospital services, or specialist community clinics. Secondary care services are usually obtained by patients as a result of referrals from primary care. Secondary care can be divided into two types:
Tertiary Care
Tertiary care is the highest level of specialised care. It is usually provided in large teaching hospitals (hospitals aligned to universities with medical schools). Tertiary care is for conditions that are very complex or rare, and that require the expertise of a specialist team. Some examples of tertiary care include:

NHS Eligibility for IMGs
IMGs who wish to practice medicine in the UK need to meet specific eligibility criteria. The license to practice is issued by the General Medical Council (GMC), which is the regulatory body for all doctors in the UK. The GMC also applies to all levels of registration, whether provisional, full, or on the specialist or general practitioner (GP) register.
The process of GMC registration can be complex and time-consuming, but it’s an essential step in the journey from an IMG to NHS.
To get a full registration, a candidate must have:
Once you’ve ensured that your qualifications meet the GMC’s standards, you’ll need to apply for registration with the GMC. This process includes submitting required documents as above stated which also need to undergo verification procedures, and paying the necessary fees.
After successfully obtaining registration, you can apply for a license to practice, which involves additional assessments and checks conducted by the GMC. The GMC website has information about applying to join the register to help you assess the type of registration you may be eligible to apply for.
Exams & Assessments
Unless you are sponsored for a UK fellowship or the MTI scheme, you will need to have passed the PLAB exams or complete the exams for membership of a Royal College (such as MRCP, PACES, MRCEM, or FRCA Primary). If you’re keen to pursue a career in a specific speciality, it might be worth taking on the challenge of the membership exams before you move to the UK. However, these are traditionally more difficult than the PLAB exams and are probably more appropriate for those who have experience in speciality.
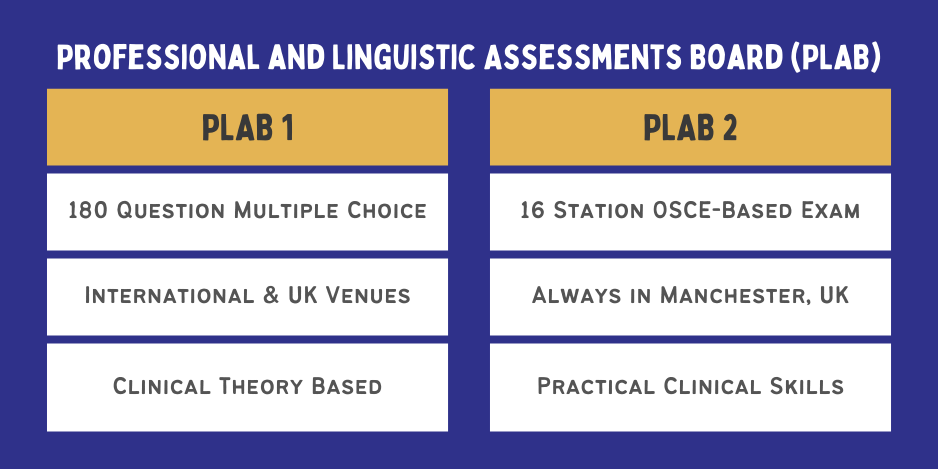
If you opt for the PLAB route, after clearing English Proficiency Test, you will be required to pass the Professional and Linguistic Assessments Board (PLAB) exams to demonstrate your clinical knowledge and skills.
It has two parts:
PLAB 1
PLAB 1 is an exam to assess theoretical medical knowledge. You’ll need to answer 180 multiple-choice questions involving clinical scenarios within 3 hours. These exams can be taken outside of the UK in one of the international exam locations, or in the UK.
The PLAB 1 exam tests clinical theory, specifically looking for your ability to diagnose and treat conditions according to NICE guidelines or within NHS systems. There are plenty of exam resources available for PLAB 1, including question banks, books, and courses.

PLAB 2
This is the second and final part which is more like an in-person OSCE exam. You’ll be given “real-life” scenarios in different care settings. There will be simulators who will act like real patients and you will be marked based on your overall consultation.
Typically, Markings are given under 3 domains; Data gathering, Interpersonal Skills, and Management. Communication skills are key to this exam, and are heavily emphasised in UK medical practice.
PLAB 2 is examined at locations in Manchester, UK, and cannot be taken abroad. There are plenty of PLAB 2 resources available, including a few PLAB courses also based in Manchester, to give you the final push you need to pass the PLAB first time.
Is PLAB doable?
Absolutely. All you need is to be a “Safe Doctor”; this is what NHS is looking for.
The PLAB route is sometimes frustrating and difficult, but if you choose the right resources and spend time studying and practising, you should be able to pass these without too many issues.
The UKMLA
The planned introduction of the United Kingdom Medical Licensing Assessment (UKMLA) around 2024-2025 is a significant change in the assessment process for both UK graduates and international graduates pursuing a medical career in the UK. The UKMLA will now be mandatory for medical students in the UK who want to join the register.
While the PLAB will be changing slightly to align itself with the UKMLA content map, IMGs will still be taking the PLAB exams. The PLAB 1 will align with the Applied Knowledge Test (AKT), and the PLAB 2 will align with the Clinical and Professional Skills Assessment (CPSA).
The proposed pattern of the exam is as below:
Applied Knowledge Test (AKT):
- Computer-based examination
- Will be conducted four times a year.
- While UK medical students will take the exam in their respective schools, IMGs will have the opportunity to take the similar PLAB 1 at select locations around the world.
- Similar to PLAB 2 exam.
- Will be taken at GMC Clinical Assessment Center located in Manchester.
The introduction of the UKMLA reflects the commitment of the UK medical regulatory body to maintain high standards of medical practice and ensure patient safety.
By implementing a unified licensing assessment for both UK graduates and international graduates, the GMC aims to create a level playing field and establish a comprehensive evaluation process that encompasses both knowledge and practical skills.
So when the UKMLA becomes fully implemented, it will play a pivotal role in shaping the future of medical practice in the United Kingdom.
VISA
Once you obtain your registration, you are good to go for applying for jobs.
To work in the UK as an IMG, you’ll need to obtain an appropriate visa. The most common visa route for doctors is the Tier 2 (General) visa. This involves securing a job offer from an NHS trust or a recognised sponsor, meeting specific eligibility criteria, and obtaining a Certificate of Sponsorship (CoS).
It’s crucial to consult the UK Visas and Immigration website or seek professional advice to ensure you meet all the requirements. Check the UK Government’s website to find out more.

Working in the NHS
Recruitment
The recruitment process within the NHS follows a structured approach. Various medical positions are advertised through online platforms, NHS trust websites, and medical journals.
Before applying you must work on building up your portfolio. A nicely organised and presented CV will keep you well ahead in the race.
Candidates are required to submit applications, which are then shortlisted based on qualifications and experience. Shortlisted applicants are invited for interviews and assessments, where their skills, knowledge, and suitability for the role are evaluated.
Salary
Salaries for doctors in the NHS vary depending on factors such as experience, speciality, and location.
As a junior doctor, you can expect to start at a Foundation Year 1 level, with salaries typically ranging from £28,243 to £32,691 per annum. As you progress through training and gain experience, your salary will increase accordingly.
If you are applying to a senior clinical fellow job, or are planning to work as a GP or consultant, you can expect your salary to follow a similar scheme to UK-trained doctors in similar jobs.
You can also earn extra income by applying for shifts at your local trust through the NHS bank system, or by working as an external locum at another trust. External locum opportunities pay better, however, if you are on a Health and Care Worker visa you will only be permitted to work an extra 20 hours a week maximum.
Working Conditions and Benefits
Doctors in the NHS enjoy several benefits and reasonable working conditions. The NHS provides a supportive work environment with access to advanced medical technology and resources.
Work-life balance is emphasised, and there are policies in place to ensure safe working hours (maximum 48 hours per week on average), including the ability to exception report overtime and missed breaks if you are a trainee, and the chance to work less than full time.
Additionally, doctors receive extensive benefits packages, including competitive salaries, annual leave, and pension schemes. The pension scheme in particular is noted to be one of the best in the UK.
Access to professional development opportunities is good, with some training programmes and fellow jobs including a study budget and study leave allocation for courses, study, and conferences.
With all this said, however, it’s important to note that trainees have noted increasingly difficult conditions, increased stress and burnout, and worsening pay over time. This is an ongoing political issue which may improve over time, however, and you may still find that UK conditions are more beneficial than the alternatives.

Career Pathways for IMGs in the NHS
The NHS offers diverse career pathways for doctors. You can choose to specialise in a specific area such as general practice, surgery, psychiatry, paediatrics, or radiology, among many others. Additionally, you can pursue leadership roles, academic positions, research opportunities, or even undertake clinical fellowships and international exchanges.
It’s important to note that the specific pathway and requirements may vary depending on your chosen speciality, individual circumstances, and the current policies and regulations of the NHS. It is advisable to consult with the relevant regulatory bodies and speciality training programs for detailed information and guidance tailored to your situation as an IMG.
Let’s shed light step by step…
Non-Training Jobs
If you have done an internship year in your current country and wish to get a job that doesn’t require training, or move to speciality training without following the foundation programme, non-training jobs are an option.
These jobs can be applied for and will see you working on a contract with an NHS trust at either SHO (senior house officer) or SpR (registrar) level. Quite often, these jobs are referred to as “junior clinical fellow” (SHO grade) and “senior clinical fellow” (SpR grade).
These jobs won’t include as much opportunity for time away from service provision to learn but can pave your way towards training programmes and may have less competition than a typical training job.
Training Jobs
Foundation Programme
The Foundation Program is the gateway to success in the dynamic world of healthcare for newly fresh graduates. It is designed to bridge the gap between medical school and independent clinical practice.
This structured scheme comprises foundation training lasting two years. If you are yet to complete an internship year, you will be required to start at Foundation Year 1 (FY1). However, if you have completed 12 months of the equivalent of foundation year 1 in your current country, you can start at the FY2 level.
Following completion of the FY programme, you will gain foundation competency and become eligible for speciality training.
Responsibilities :
FY1 and FY2 doctors work closely with consultants, senior doctors, nurses, and other healthcare professionals in a multidisciplinary team. In a nutshell, Effective teamwork and collaboration are the mainstays of providing optimal patient care in NHS!
Speciality Training Programmes
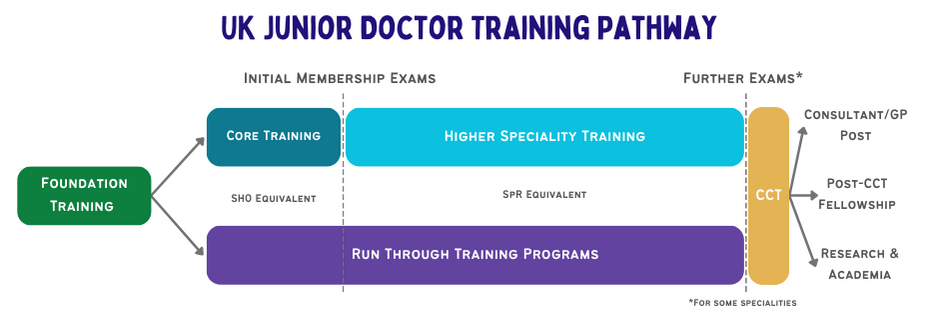
Speciality training programmes bridge the gap between foundation-level doctors and completion of a CCT certificate in order to become a consultant. These programmes can initially be applied to if you have gained competencies via the foundation programme, though if you have completed an internship year in your current country there are a few options:
Speciality training programmes post-foundation take the form of either Core Training Programmes (2-3 year CT programs that lead on to 3-5 year higher speciality ST programmes) or run-through Speciality Training programmes (5-8 year programs that will take you to the level of a consultant).
You will need to pass professional examinations to progress to higher speciality training. The most common examinations are the Membership of the Royal Colleges of Physicians of the United Kingdom (MRCP UK) and the Membership of the Royal College of Surgeons (MRCS). Which exams you take will depend on your chosen speciality.
General Practice Training (GPST)
If you are interested in pursuing a career in general practice, you can apply for the General Practice Training program. This programme is different from most CT/ST programmes in that it takes only 3 years to complete if working full time.
The GPST programme includes rotations in different settings including acute care, mental health, and primary care. Following this programme you become a fully qualified general practitioner and can work as a salaried, locum, or partnered GP.
Other Career Paths
Academic Pathway
If you have a keen interest in research and academia, you can explore academic pathways within the NHS. This may involve undertaking a PhD or pursuing research fellowships to develop expertise in a particular field.
Academic careers often involve a combination of clinical work and research.
Speciality Fellowship
Some IMGs may choose to gain additional experience and expertise by pursuing speciality fellowships. These fellowships provide advanced training and focus on specific sub-specialities within a particular medical discipline.
Fellowships can range from one to three years and offer an opportunity to enhance clinical skills and knowledge.
Clinical Leadership and Management
If you have an interest in healthcare leadership and management, you can pursue opportunities in clinical leadership roles or healthcare management positions. These roles involve overseeing clinical services, quality improvement, and strategic planning within healthcare organisations.
How Does the NHS handle CPD?
The NHS places significant emphasis on CPD for doctors. It encourages doctors to engage in lifelong learning, attend conferences, participate in workshops, and pursue postgraduate qualifications. The NHS supports doctors’ CPD through dedicated training budgets, study leave allowances, and access to online learning resources.
Doctors in non-training jobs will be required to log a certain number of CPD hours per year in order to be revalidated by the GMC, though trainees will take part in CPD activities without the requirement for logging hours.
Challenges Faced by IMGs
IMGs working in the NHS may encounter challenges associated with working in a new country. Integration into a new work environment and establishing professional networks may also require extra effort. Here are some common challenges that IMGs may encounter:
Professional Challenges
Language and Communication
Language proficiency can sometimes be a significant challenge, as effective communication with patients, colleagues, and other healthcare professionals is crucial for providing quality care. Adjusting to the nuances of the English language, accents, and medical terminologies may require extra effort and practice.
Professional Recognition and Registration
IMGs must go through a process of professional recognition and registration. This process can involve rigorous assessments, examinations, and documentation requirements, which may pose challenges for some IMGs.
Professional Development and Career Progression
IMGs may encounter additional requirements and expectations for career advancement within the UK healthcare system. Meeting professional development requirements, pursuing speciality training, and understanding the pathways for career progression may require thorough research and planning.

Cultural Challenges
Cultural shock refers to the feelings of disorientation, confusion, and anxiety that individuals may experience when they are exposed to a new culture or environment that is significantly different from their own.
Being an overseas doctor cultural shock can be a common experience to navigate the healthcare system and adapt to the British culture.
Work Culture
The work culture in the UK, including the NHS, may differ from what IMGs are accustomed to in their home countries. Different expectations regarding hierarchy, teamwork, decision-making processes, and work-life balance can contribute to a sense of culture shock.
It may take time to understand and adapt to these cultural nuances.
Professional Practices
Medical practices and protocols may vary across countries. You may need to familiarise yourself with the specific guidelines and protocols followed in the UK, including documentation practices, patient management, prescribing medications, and ethical considerations.
A great place to start learning guidelines (including diagnosis, treatment, and referral) is the NICE website.
Healthcare System
The structure and organisation of the healthcare system in the UK, particularly the NHS, can be complex and different from the systems in other countries.
Understanding the referral pathways, administrative processes, healthcare policies, and the role of various healthcare professionals can be overwhelming at first.
Social and Cultural Differences
IMGs may encounter social and cultural differences in social norms, traditions, religious practices, dietary habits, and lifestyle choices. Adapting to these differences can take time.
There is also plenty of cultural communication differences hidden within British slang, including tone, humour, and sarcasm.
Discrimination and Bias
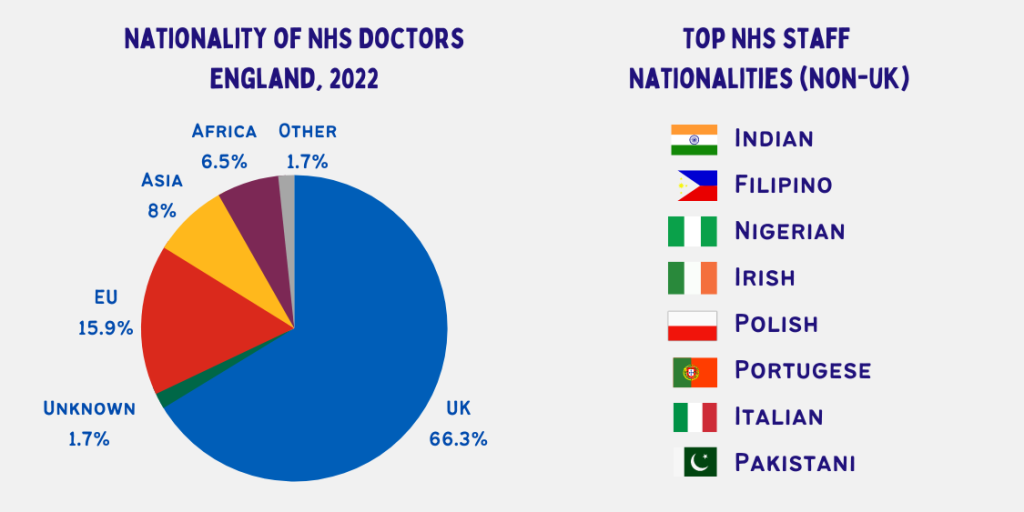
Unfortunately, some IMGs may face discrimination or bias in the workplace due to cultural or ethnic differences. The NHS is a very multicultural organisation, with around 1/3 of NHS doctors originating outside the UK, and plenty of diversity within the British-national doctors of the NHS.
Moving Past Culture Shock
Overcoming cultural shock is vital for IMGs to develop cultural competence, provide patient-centred care, communicate effectively, adapt professionally, ensure personal well-being, advance their careers, and gain a global perspective.
It’s also important to note that culture shock is a temporary phase, and with time, patience, and open-mindedness, IMGs can overcome these challenges.
Here are some tips to help you overcome culture shock when you move to the UK:
1. Educate Yourself
Take the time to learn about the culture, customs, traditions, and social norms of the country or community you are entering. Understanding the local culture will help you negotiate and adapt more easily.
2. Maintain an Open Mind
Embrace the differences you encounter and approach them with curiosity rather than judgment. Recognise that cultural diversity brings new perspectives and opportunities for growth.
4. Communicate and Connect
Seek opportunities to interact with locals, colleagues, and other IMGs to build relationships and understand their experiences. Engage in conversations, ask questions, and listen actively to gain insights and forge connections.

5. Seek Support
Reach out to support networks or mentorship programs specifically designed for IMGs. Connecting with others who have gone through similar experiences can provide guidance, reassurance, and practical advice.
6. Be Patient
Understand that adapting to a new culture takes time. Be patient with yourself and allow yourself to make mistakes and learn from them. Gradually, you will become more comfortable and accustomed to the cultural differences.
7. Maintain Balance
Take care of your physical and mental well-being. Activities like social gatherings or charity work might help you revive and feel relaxed. Balancing work and personal life will contribute to a smoother transition and better overall adjustment.
8. Celebrate Similarities and Differences
Recognise and appreciate both the similarities and differences between your own culture and the new culture. Finding common ground will help you connect with others while appreciating differences will foster mutual respect and understanding.
Remember that overcoming cultural shock is a personal journey, and it’s normal to experience a range of emotions during the process. By embracing the challenges and seeking to understand and adapt, you can navigate cultural shock successfully and thrive in your new cultural environment.

The Best Support Networks and Resources for IMGs
The NHS acknowledges the importance of support for IMGs and provides various resources and networks. Support networks and resources available for International Medical Graduates (IMGs) within the NHS can vary depending on the specific region and organisation. You should inquire with your employers or relevant professional bodies to access the most up-to-date information on available support networks and resources in your specific area of practice.
Here are some common support networks and resources that IMGs may find helpful:
There are several associations and organisations specifically dedicated to supporting international doctors within the NHS. Examples include the British International Doctors’ Association (BIDA).
Some regions or organisations within the NHS offer specific training programs or fellowships for IMGs. These programs provide additional support and training opportunities to help you adapt to the UK healthcare system.
This includes schemes such as the Medical Training Initiative.
These programs provide an overview of the NHS system, its policies, and procedures, and help you to understand your roles and responsibilities.
Some employers may sign you up for the new NHS Induction Programme on e-lfh.
Various training programs, workshops, and conferences are available so that you can join and enhance clinical skills, knowledge of NHS systems, and understanding of UK healthcare regulations.
These programs pair you with experienced healthcare professionals who can provide guidance, advice, and support throughout your transition into the NHS.
IMG mentors can be UK-trained doctors or other IMGs who have experienced all of the challenges that you face.
Recognising the importance of cultural differences and language barriers, some NHS organisations provide cultural awareness training and language support for IMGs. These resources can help you understand UK cultural norms, improve language proficiency, and effectively communicate with patients and colleagues.
Employee Assistance Programs (EAPs) are available in some NHS organisations. These programs offer confidential counselling and support services to help healthcare professionals, manage personal and work-related challenges, stress, and mental health issues.
Online platforms and forums can be your near-at-hand resources within the NHS. Websites, social media groups, and discussion forums specific to IMGs provide a platform for sharing experiences, seeking advice, and connecting with others who have gone through similar transitions.
Examples include Facebook groups (such as the Scottish IMG Doctor Support Network) and support organisations like the Doctors Support Network.
It’s important to note that the availability of specific support networks and resources may vary by region or NHS organisation. You should inquire with your employers or relevant professional bodies to access the most up-to-date information on available support networks and resources in your specific area of practice.

Conclusion
In conclusion, an aspiration to work in the UK is an exciting and achievable dream that holds immense potential for personal and professional growth. With its thriving economy, diverse job opportunities, and vibrant cultural landscape, the United Kingdom offers a fertile ground for individuals like IMGs to flourish in their chosen career paths.
To make this dream into a reality, most importantly, focus on thorough research about the pathway you choose. You should explore different options, the requirements, and the necessary criteria to work in the UK and thus you can guide yourself on which sort of assistance you need throughout this process.
I wish you all the very best in paving the way for a successful and rewarding career in the NHS!