Published January 28, 2023 | Updated June 11, 2024
By Jaimin Arya
Jaimin is an ST5 Anaesthetic Registrar based in East Midlands. He has experience working in both London and East Midlands, and runs anaesthetic interview courses for CT1 and ST4 level entry
Core and ACCS Anaesthetics interviews have always been highly competitive, but in the round 1 application, you’ll be competing with more applicants than ever before!
This is no surprise given that anaesthetics core training has a reputation as a well-supported training programme.
In the past couple of years, the competition ratio for anaesthetics recruitment has risen by over 60% to 4.78 in 2023. This means that when you apply, you’re competing with 3 (point one nine) others for the place!
While a good MSRA score will get you through to the interview stage and contribute towards 15% of your final score, this isn’t enough to guarantee you a place for either CT1 or ACCS anaesthetics; you also need to prepare well for the interview.
In this article, we’ll go through the Core and ACCS Anaesthetics interview process, giving you plenty of tips to help you perform at your best.
Hints and Tips by Dr Jaimin Arya
Jaimin is an ST5 Anaesthetic Registrar based in East Midlands. He has experience working in both London and East Midlands.

Having gone straight through his anaesthetic training, getting his first choice for registrar jobs and having passed his FRCA in ST4 he Is perfectly placed to help optimise your anaesthetic application and CV.
Jaimin is the founder of The London Anaesthetic Interview Course, which helps CT1 and ST4 candidates obtain their perfect job in anaesthetics.
On the CT1 course, aimed at both Core and ACCS anaesthetics training hopefuls, previously high-scoring candidates talk you through the structures and blueprints for the interview, which is followed by 1-to-1 mock interviews.
Key Documents
Want to Learn More About ACCS?

The Core & ACCS Anaesthetics CT1 Interview Process
The core anaesthetics interview is the final hurdle for trainees hoping to start their careers via either the Core OR ACCS anaesthetics pathways, with both of these pathways recruiting via a single application and interview process.
If you’re still undecided at this point whether you’d prefer to join the core training or ACCS pathway, you still have time to decide before you choose your preference. For more information, check out our Ultimate Guide to ACCS Training.
All CT1 Anaesthetics interviews will be held online in 2024, with no suggestion that this will change at any time in the future.
Shortlisting for the interview is done via the MSRA exam, whereby candidates who have managed to achieve an MSRA score above the cutoff (determined by the interview capacity) will be invited to interview via an email with instructions on how to book your interview on Oriel.

When invited to interview, you will be allocated to an online interview in the cluster you chose during the application process. Clusters include:
- Scotland
- Northern Ireland
- England & Wales (applicants must choose one nation to be considered for at this stage)
You will only receive one interview, in your chosen cluster, and you will only be considered for placements in the cluster you have chosen.
Online interviews are booked on a first-come; first-served basis, so if you have an idea if you’d prefer an early or late interview you should try to book your interview as soon as possible.
Anaesthetics Interview Timeline
We’re still awaiting information from ANRO on the specific Anaesthetics Round 1 2024 application key dates. These dates are from HEE and the interview dates may vary according to speciality (within the 2 Jan to 22 March limits)
| Applications open | Thursday 26th October 2023 at 10am |
| Applications close | Thursday 23rd November 2023 at 4pm |
| MSRA window | Thursday 4th January – Sunday 14th January 2024 |
| Invitation to Interview | Wednesday 14th February 2024 |
| Interview Acceptance Deadline | Friday 16th February 2024 at 4pm |
| Interview window | Monday 26th February – Friday 8th March 2024 |
| Initial Offers out | Monday 25th March 2024 by 5pm |
| Hold deadline | Thurs 4th April 2024 at 1pm |
| Upgrade Deadline | Tuesday 9th April 2024 at 4pm |
| Post start date | Wednesday 7th August 2024 |
Jaimin’s Tips – When Should I Start Preparing?
Start practising early! As soon as you know you have an interview start practice with whoever is available, it doesn’t even have to be from the medical field.
Try an attend courses (such as The London Anaesthesia Course!), practice with colleagues and approach anaesthetic trainees at your local hospital who may be willing to help too! We are a friendly bunch.
Have a look at the scoring matrix on the ANRO website, it gives you an idea of how they score these interviews. This will allow you to tailor your practice to ensure you get the most amount of points from your answers.
The CT1 Anaesthetics Interview Format
The online interview will take a total of 30 minutes in length, with two sections lasting 15 minutes each – a clinical scenario and a general interview. You won’t be given any questions in advance of the interview day, but both sections use a scoring guideline which gives us an idea of the questions that might be asked.
Interview Day – Performing at Your Best
Interview day is full of indomitable nerves and last-minute crises, with a sprinkling of self-doubt. To prevent a complete breakdown on the day you need to prepare in advance:
Get Your Sleeping Pattern Right
It will already be difficult to sleep on the night before the interview, and with a poor sleeping pattern, it may become nigh-on-impossible. Set a regular alarm and bedtime and stick to it for at least a week before the exam.
Book some leave.
A last-minute night shift will mess up both your interview preparation and your sleep cycle. Try to book some leave in the days leading up to the interview.
Don’t wear yourself out.
Your mental state can turn a decent interview into a car crash – don’t burn yourself out by fitting incessant revision and practice around your work! Book a spa day, chill out in the bath, or do something else that relaxes you – there is such a thing as too much prep.
Prep your tech.
Remember all of the zoom-based shenanigans during early-lockdown teaching days? This might be amusing to zoom-room full of foundation docs but is less so to interviewers. Make sure your webcam, microphone, and internet are all running smoothly on the day.
For each section, you will have two assessors, so four in total. Each assessor marks your interview separately and will give you a global rating in addition to the other scoring domains.
Let’s go through the two sections of the interview and the potential questions.
Section 1 – Clinical Scenario
Section time: 15 minutes
The clinical scenario section assesses your knowledge and ability to problem-solve. You will be given 2 minutes to look at a clinical scenario, take notes and consider how you might answer questions, after which the interview will officially start.
You will then have 15 minutes in which to answer questions about the clinical scenario from your assessor, discussing how you would approach your assessment, investigation, and management of the patient.
This section of the interview is looking at the “Clinical skills – clinical knowledge and expertise” part of the CT1/ACCS anaesthetics person specification, which includes:
- Your ability to apply sound clinical knowledge and judgement to problems.
- Your ability to prioritise clinical needs.
- Your ability to maximise safety and minimise risk.
- Your recognition of, and ability to undertake the initial management of, an acutely ill patient.
You are not expected to have detailed knowledge of anaesthetics when applying, so the clinical scenario is likely to be a common situation or emergency that a foundation year 2 doctor should be able to deal with.
The point of the clinical scenario is to assess your decision-making, team working, reflection, and working under pressure – note these domains are not entirely dependent on your clinical knowledge.
Your assessors are trying to work out whether their patients are in safe hands and whether you will function well as a core anaesthetic trainee:
- Is your approach to an emergency safe and systematic?
- Can you initiate management appropriately?
- Are you able to judge when to escalate to a senior?
- Will you stay calm in an emergency?
An ABCDE approach to the scenario is advisable but regardless of your approach, you should always have a structure to fall back on. Losing your head due to nerves and adrenaline is a common experience, but if you have a structure in place to fall back on you will always have somewhere to start again.
Here’s an example of an emergency scenario that you might be expected to answer:
Example Clinical Scenario
“You are a Foundation Year 2 doctor working out-of-hours as the overnight on-call surgical SHO. A staff nurse from the general surgical ward calls to inform you that he is concerned about one of his patients.
He tells you that his patient is a 57-year-old female who underwent an emergency laparotomy earlier in the day for small bowel perforation. He reports that his patient is drowsy and looks unwell, pale, and clammy.
Please explain how you would approach this scenario.”
In the above scenario, you have been called to an acutely unwell patient and must demonstrate to your interviewers that you can make sensible treatment and escalation decisions. This is a roleplaying exercise, and you must imagine what you would do in this situation.
As a first step, it may be wise to gather further information on the scenario. To prioritise your jobs, you must ascertain how unwell this patient is. Pertinent questions might include what the patient’s observations are, whether there were any complications during their procedure, and what the patient’s GCS is.
Once you have your answers, you must decide how urgent treatment should be. You could consider:
- Is there anything you should ask the nurse to do while on the phone (such as further observations or interventions such as cannulation)?
- Are there any immediate interventions which need to happen (such as a cardiac arrest 2222 call or fast-bleep to a senior)?
- How should you prioritise attending the surgical ward?
As you go along in this scenario, your interviewers will try to give you the requested information and provide further prompts as you work your way through the diagnosis, investigation, and treatment of the patient. Scenarios are likely to be familiar to anyone who has worked as a foundation doctor.
Further questions that your interviewer might ask as you go through the scenario include:
- “How would you assess the patient?”
- “What is your differential diagnosis?”
- “Are there any immediate treatments you would start at this point?”
- “What investigations would you request?”
- “Would you like to contact anyone at this stage?”
- “How would you explain the situation to the patient?”
- “How would you prioritise this compared to X and Y?”
The potential questions on this are limitless, but you can see that most of these questions will be related to your everyday practice. You should aim to answer these questions calmly, concisely, and with structure.
Jaimin’s Tips – Clinical Scenario
The amount of anaesthetic knowledge they will expect of you will be negligible. They want to know you are a safe pair of hands, sensible and know your limitations.
The A-E approach will always come in handy. Make sure you practice this and can recite this in your sleep!
Other all-time favourites will be questions on managing workload, prioritising cases, and dealing with emergency situations. Come up with examples of when you have been a part of these situations.
Remember in your experience where these scenarios worked well and not so well? Think through why they did they worked. This will give you a lot of material on how to answer these questions.
They want to see you can stay calm and not panic under questioning. When was the last time you went to an arrest and saw an anaesthetist flap and panic?!
Section 2 – General Interview
The general interview section of the interview also lasts 15 minutes, and is essentially the “portfolio station”. Within this section your interviewers will be assessing:
- Commitment to Speciality
- Qualifications
- Involvement in Teaching, Quality Improvement, Audits, and Research
- Reflective Ability
Each section is an opportunity to shine, emphasising anything you’re particularly proud of and helping to demonstrate that you are a well-rounded doctor. Each of these scoring domains is marked by both assessors out of 5 (for a total of 10 points).
When preparing for the interview, go through your portfolio to eke out your most impressive achievements. While you should avoid reeling off a list, it’s still important to be concise in your answers, as there is a lot to cover in this section.
Though the portfolio is no longer used for scoring (after being usurped by the MSRA exam), the defunct and outdated self-assessment criteria can still guide you to which of your experiences might prove more valuable to discuss in detail.
Jaimin’s Tips – General Interview
Remember these questions are ones you would have come across in your practice so keep calm and cool!
As I previously said make sure you have a different example for each domain they assess in the interview. It shows how good a CV you have as well as how well you can answer the question. Two birds with one stone!
Think early about how you can answer the standard questions such as ‘Why anaesthetics’ differently. You want to stand out from the crowd and have a unique answer that the interviewers will remember… In a good way!
Finally, there are 20/100 marks for a global rating for both parts of the interview- So being nice, and polite and having well-structured and confident answers go a long way!
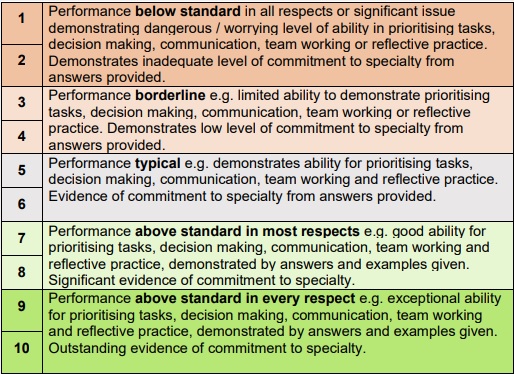
Interview Scoring
The maximum available interview score is 120, with the two stations making up 40 of the marks each, and the final 40 marks being awarded by assessors as a “global rating”.
The minimum score required to be considered appointable is 64/120. If you score below this, you will not be considered appointable and will not be considered for a training post.
If you have a particularly poor performance in the interview, and one or more assessors have decided that you should be vetoed out of the process, your case will be discussed with the clinical lead and a decision made about whether you should be considered appointable. If all four assessors agree that you should be vetoed, you will automatically be removed from the process.
The scoring for each station is as follows:
Clinical Scenario Scoring (40 marks)
Four scoring domains, scored out of 5 by both assessors (for a total of 10 marks per domain)
- Decision Making
- Reflective Practice
- Team Working
- Working Under Pressure
Clinical Judgement & Decision Making
| 5 Points |
| o Comprehensive understanding of the needs of the situation. o Seeks team input, asking for appropriate help. o Always alert to signs and symptoms which might destabilise the patient. o Regularly reviewed the situation and prioritised tasks appropriately. o Excellent planning and took decisive and appropriate action. |
| 3 Points |
| o Good understanding of the needs of the situation. o Noticed significant changes to the clinical situation. o Regularly reviewed the situation. o Some evidence of structured thinking and planning. o Firm idea of appropriate solutions to problems. |
| 1 Point |
| o Poor understanding of the needs of the situation. o Lack of urgency and decisive action. o Failed to notice significant changes in the clinical situation. o Disorganised approach to patient assessment. o Lack of forward planning and structured thinking. o Unable to suggest workable solutions to the problem. |
Scores of 2 or 4 are given for candidates who fit somewhere between these descriptions.
Team Working
| 5 Points |
| o Ensured team capabilities matched task, escalating appropriately. o Always confirmed understanding and instructions. o Clear communication of plans. o Sympathetic and considerate of other team members. o Showed leadership with authority and justification. o Always participative with a non-confrontational approach. |
| 3 Points |
| o Showed awareness of team capabilities, escalating appropriately. o Negotiated and compromised with team members. o Good rapport with team. o Delegated tasks appropriately. o Maintained non-confrontational approach. |
| 1 Point |
| o Lack of awareness of team capabilities. o No understanding of the needs of team members. o Rude, confrontational, or critical of team members. o Failed to delegate tasks or show leadership. o Failed to escalate appropriately, undertaking tasks outside level of competence. |
Scores of 2 or 4 are given for candidates who fit somewhere between these descriptions.
Working Under Pressure
| 5 Points |
| o Relaxed and comfortable with the situation. o Responded quickly to unexpected changes. o Always maintained perspective. o Flexible and open in manner when challenged. o Aware of personal limitations and of when tasks are outside their level of competence. o Effectively dealt with other’s opinions and questions. |
| 3 Points |
| o Remained calm for most of the scenario. o Took decisive action. o Maintained perspective. o Some flexibility when challenged. o Insight into personal limitations. o Listened and responded to other’s opinions and questions. |
| 1 Point |
| o Tense and agitated. o Hesitant to take decisive action. o Focussed on immediate worries without maintaining perspective. o Rude or offensive when challenged. o Unable to adapt to changing situations. o Disregarded other’s opinions and questions. |
Scores of 2 or 4 are given for candidates who fit somewhere between these descriptions.
Reflective Practice
| 5 Points |
| Educational Appraisal o Evidence of regular educational appraisal with clear outcomes from meetings. o Gives examples of how these appraisals affected professional development. Risk Management o Describes engagement in reducing risk in the workplace through critical incident reporting or meetings. o Shows insight into the impact of non-technical skills on the delivery of service in the NHS and mitigation of recognised issues. Personal Development Plans (PDPs) o Accounts for the content of Foundation Personal Development Plans in curriculum and other outcomes. o Shows how PDPs enable career planning and demonstrate commitment to speciality. Assessment Tools o Describes a minimum of 2 workplace assessments and evidence of how these have been used for practice and personal development. o WPA’s include TAB/MSFs, education supervisor meetings, self-audit, mini-CEX, case-based discussion (CBD), procedure logs, DCTs, and reflections. Feedback o One or more examples of feedback which resulted in behavioural change, improved outcomes, or career development. |
| 3 Points |
| Educational Appraisal o Describes how educational appraisals have been used in professional development. Risk Management o Describes personal non-technical skills role in clinical risk management. Personal Development Plans (PDPs) o Accounts for content of Foundation Personal Development Plans in curriculum and other outcomes. Assessment Tools o Describes workplace assessments and how these have been used to change personal clinical practice. Feedback o One or more example of feedback which resulted positive professional change. |
| 1 Point |
| Educational Appraisal o Unable to give examples of how educational appraisal has affected professional development. Risk Management o Limited description and understanding of clinical risk management and personal non-technical skills. Personal Development Plans (PDPs) o Limited evidence of appropriate PDPs. o Unable to link these to professional development. Assessment Tools o Limited description of how WPA’s were used to enhance professional development. Feedback o Little evidence of feedback used to change practice or improve outcomes. |
Scores of 2 or 4 are given for candidates who fit somewhere between these descriptions.
General Interview Scoring (40 marks)
Four scoring domains, scored out of 5 by both assessors (for a total of 10 marks per domain)
- Commitment to speciality
- Involvement in Teaching, Audit, QI, Research
- Reflective Practice
- Qualifications & Experience
To give you an idea of what is expected of you in each scoring category, we have written a summary of the guidance given to assessors. You can find the full and official descriptions on the ANRO website.
Qualifications and Experience
| 5 Points |
| o Excellent description of the below. o Meets qualifications required in person specification. o Additional qualifications related to anaesthesia (PGCert/Dip, additional degrees). o Good experience relevant to anaesthesia such as taster days and placements. |
| 3 Points |
| o Adequate description of the below. o Meets qualifications required in person specification. o Some experience relevant to anaesthesia. |
| 1 Point |
| o Unable to describe suitable qualifications and experience. |
Scores of 2 or 4 are given for candidates who fit somewhere between these descriptions.
Teaching, Audit, Quality Improvement, and Research
| 5 Points |
| o Excellent description of the below. o Significant teaching experience and/or teaching qualifications. o Clear insight into the role of the anaesthetic trainee as educator. o Major involvement in QI, research, and/or audit with significant change made. |
| 3 Points |
| o Adequate description of the below. o Some teaching experience and/or teaching qualifications. o Some insight into the role of anaesthetic trainee as educator. o Involvement in QI, research, and/or audit with limited change made. |
| 1 Point |
| o Limited description of suitable teaching, QI, audit, or research experience. |
Scores of 2 or 4 are given for candidates who fit somewhere between these descriptions.
Commitment to Speciality
| 5 Points |
| o Excellent knowledge of the anaesthesia/ACCS training programme. o Career plan with clearly defined strategy to maximise training opportunities. o Good evidence demonstrating intention to follow career in anaesthesia. |
| 4 Points |
| o Good knowledge of the anaesthesia/ACCS training programme & how to maximise training opportunities. o Some evidence of intention to follow career in anaesthesia. |
| 3 Points |
| o Some knowledge of the anaesthesia/ACCS training programme & how to maximise training opportunities. |
| 2 Points |
| o Limited evidence of knowledge of the anaesthesia/ACCS training programme o Limited insight into a career in anaesthesia. |
| 1 Point |
| o No evidence of knowledge of the anaesthesia/ACCS training programme. o No insight into a career in anaesthesia. |
To hit maximum points and show excellent evidence of knowledge in these domains, you should aim to demonstrate:
- Commitment to speciality – give evidence of experience in anaesthesia, such as on undergrad/postgrad placements, taster days, and career days.
- Insight into anaesthesia – demonstrate that you understand what a career in anaesthesia looks like, and what your role as an anaesthetic trainee will be.
- Knowledge of the anaesthesia / ACCS training programme – show that you know how the core anaesthesia or ACCS training schemes work and that you know about the career progression to ST4.
- Career development – Demonstrate that you have put thought into how you will use the training programme to learn new skills, add to your CV, and start to create the blueprints for your future career.
Reflective Practice
This will be assessed on both stations – see above for marking.
Global Rating (40 marks)
Each assessor will then give you a mark out of 10, based on their overall impression. A score of 1 one any station is considered when the performance warrants that the candidate should be vetoed out of the recruitment process at this stage.